Though I’ve previously posted about my reversing my adrenal insufficiency, I really wanted to provide as much information as possible on this topic.
Overview of Adrenal Function
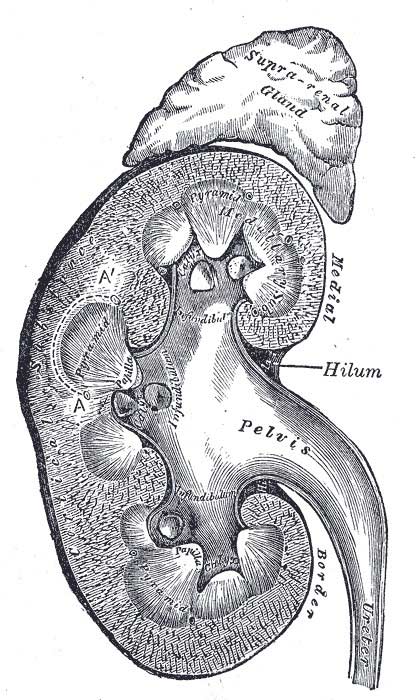
The adrenals are two small organs located just above the kidneys, consisting of an inner part (cortex) and outer part (medulla).
Overall, the adrenal glands produce 3 types of hormones: glucocorticoids (hormones that affect glucose), mineralcorticoids (hormones that affect minerals and fluid balance, i.e. electrolytes) and androgens (sex hormones).
There’s an adrenal article with much more info on Wikipedia for those who want to dive in further.
The way our bodies produce cortisol is extremely irritating to those of us who had to memorize this stuff for a biochemistry test. 😉
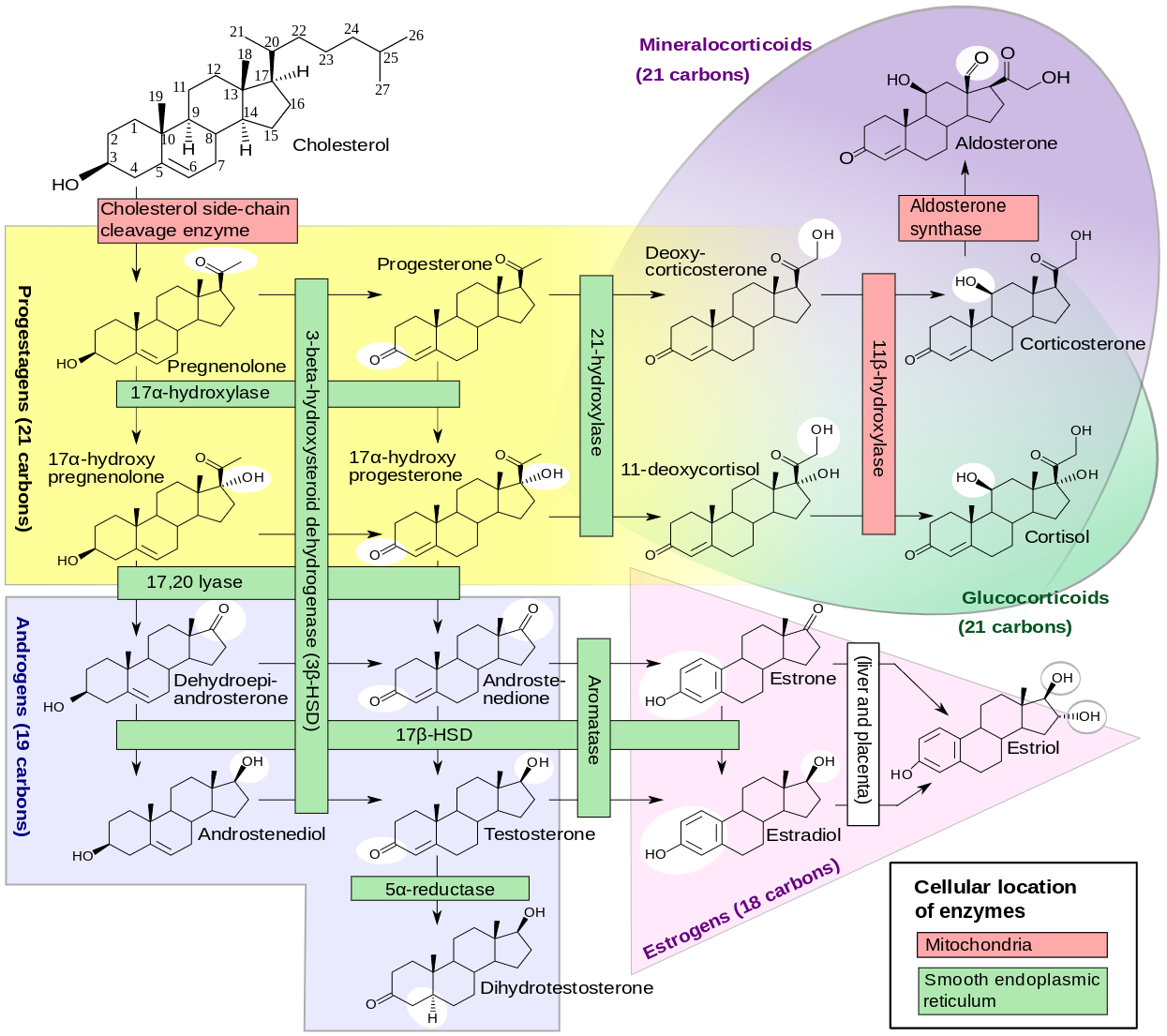 diagram of steroidogenesis from Diagram of the pathways of human steroidogenesis”. WikiJournal of Medicine 1 (1). DOI:10.15347/wjm/2014.005. ISSN 20018762. via Wikimedia Commons [CC BY-SA 3.0]
diagram of steroidogenesis from Diagram of the pathways of human steroidogenesis”. WikiJournal of Medicine 1 (1). DOI:10.15347/wjm/2014.005. ISSN 20018762. via Wikimedia Commons [CC BY-SA 3.0] less accurate, but more amusing diagram of steroidogenesis from SMBC comics by Zach Weinersmith
less accurate, but more amusing diagram of steroidogenesis from SMBC comics by Zach WeinersmithNext, I need to clear up the difference between adrenaline (ephinephrine) which is produced in the medulla and cortisol which is produced in the cortex.
I’ve seen cortisol referred to as the fight-or-flight hormone scores of times, including by doctors and others who ought to know better. Cortisol is NOT the fight-or-flight hormone, but the stress hormone.
For example, if you run into a traffic jam when you’re running late to work, you will produce more cortisol. ANY stress produces cortisol, and it can be very minor stress, e.g. your body produces cortisol before you wake up in the morning in order for you to deal with the “stress” of waking up and getting out of bed.
Adrenaline is the fight-or-flight hormone, it is the hormone produced when you nearly had a car accident and briefly thought you were going to die and are now parked on the side of the road shaking, nauseous and possibly puking. You do produce more cortisol at a time like this also, but it is not cortisol doing all that, but adrenaline.
I’ll be focusing primarily on cortisol in this article.
Is Adrenal Fatigue Real?
Mainstream Medicine Says No
For the most part, mainstream medicine recognizes two cortisol conditions, the extremes of Addison’s disease, in which you make nearly no cortisol, or Cushing’s syndrome, in which you make extreme excess amounts of cortisol.
However, just as you can have metabolic syndrome prior to developing diabetes, there is such a thing as making not enough cortisol or too much cortisol without having the recognized extreme disease states.
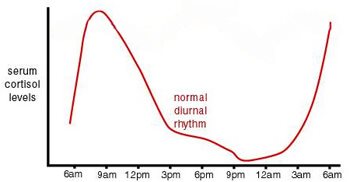
Normal cortisol production is based on a circadian rhythm, what is “normal” varies throughout the day. Shortly before you wake, cortisol peaks for the day, then gradually reduces until it’s low before bedtime. Cortisol causes the body to produce glucose, thus causing the Dawn Phenomenon, in which bG is higher on waking than it was before bed, though you have been asleep and not eating. This is the body’s way of preparing for the day.
Because cortisol raises bG and thus raises insulin, it is responsible for a certain amount of weight gain and gets a bad rap for that. You’ll often hear people talk about reducing stress to lower cortisol, but the converse is a problem also, if you don’t produce enough to get out of bed, you can be bedridden.
Further, your cortisol may be perfectly fine at one part of day and low at another time of day and high at a third time of day. Generally, if you suspect adrenal issues, most doctors will test a morning cortisol, which can have a pretty big range given it’s when cortisol amounts are changing the most. So you can be deemed “in range” and thus normal even though your cortisol production may be way out-of-whack.
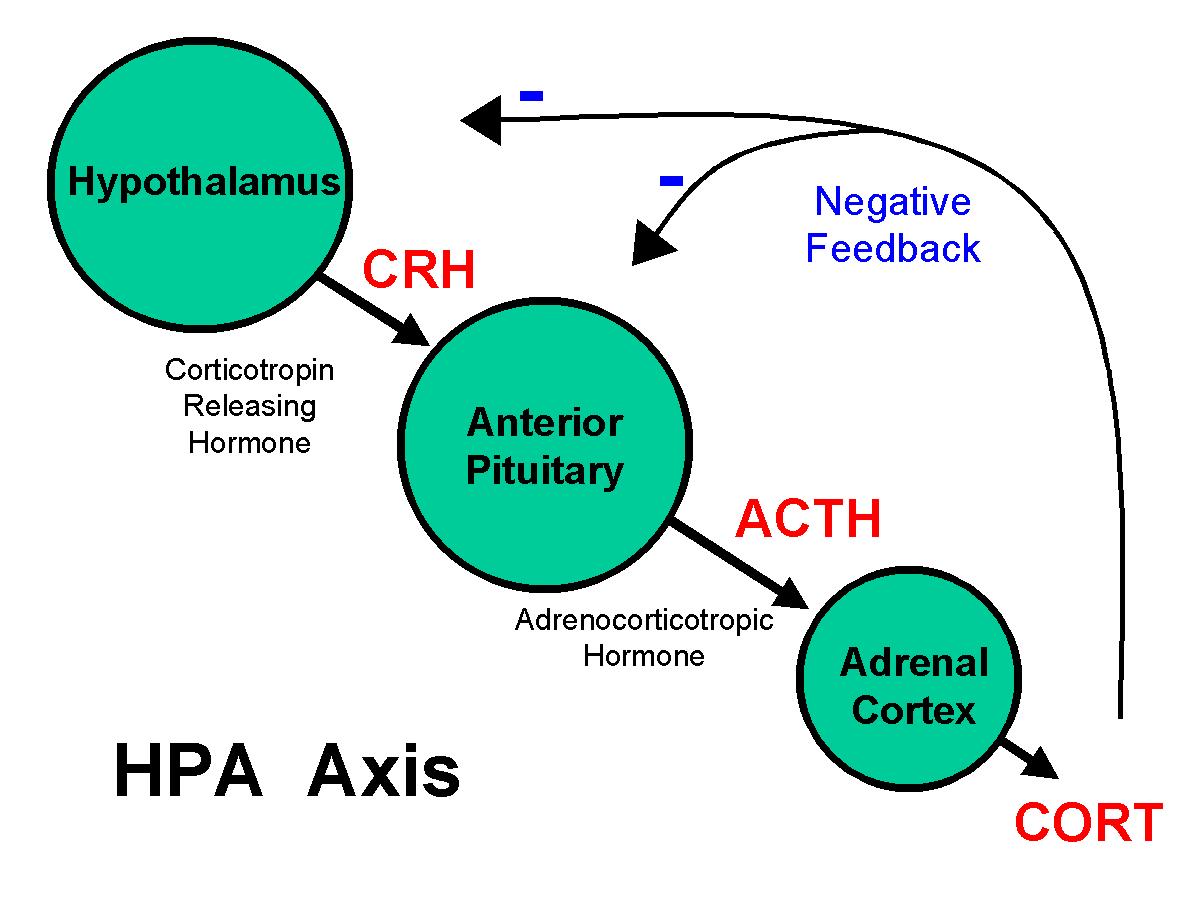
A more advanced doctor may investigate with a test called an ACTH-stim. To explain what this is I need to back up a bit.
Cortisol production is controlled by the HPA axis, the hypothalamus gland, which senses how much cortisol is available and makes a hormone to stimulate the pituitary gland, which makes ACTH, the hormone that stimulates the adrenal glands to produce cortisol under normal circumstances.
So in an ACTH-stim test, they do a blood draw, give you a shot of an ACTH analog, and then do another draw at one hour and two hours, and test cortisol at all 3 time points. Under normal circumstances, your cortisol should double at one hour and double again at two hours, proving that your adrenals can respond appropriately.
This can be useful information, but only shows if your adrenals respond appropriately to ACTH, not if there are other issues within the HPA axis that affect cortisol production. Sometimes under severe, prolonged stress, the entire HPA axis slows down or otherwise malfunctions, which has been called in common parlance “adrenal fatigue.”
Most doctors will poo-poo the notion of adrenal fatigue as a wacky alternative diagnosis, just as before bG meters were commonly available, reactive hypoglycemia was written off as a psychological issue. Generally, the medical field tends to dismiss issues it can’t test for, and refer the patient suffering them to a shrink.
Alternative Medicine
Sometimes Flaky
I personally dislike the term “adrenal fatigue” mostly because it *has* been twisted by quite a number of alternative health folks who diagnose it based on a list of vague symptoms that can be caused by any number of problems other than cortisol dysfunction.
Further, there’s a lot of ways the circadian rhythm can be messed up, being high or low at various times of day, and calling all those conditions by one name doesn’t make a lot of sense to me.
There are a few doctors (especially functional medicine doctors) who will test for cortisol throughout the day via a salivary test, during which you basically spit into a tube at 6 AM, noon, 6 PM and midnight, and the cortisol in those tubes is tested to see how it compares to a normal circadian rhythm.
This test is commonly also ordered by patients directly to check their adrenal function.
This is much more informative in figuring out what needs to be done to assist someone in correcting an abnormal rhythm.
I’ve been involved in adrenal issues for many years. My sister was born with a disease called congenital adrenal hyperplasia (CAH), odds are I carry the gene also, so I studied it in graduate school. She has never made a single molecule of cortisol in her life, and given that aldosterone is made from cortisol, she’s never made one of those either.
I found her, based on age, birthplace and such, in the medical literature as she was the second child born with CAH who survived childhood.
XX individuals born with CAH have been exposed to excess testosterone prenatally, but not enough to develop as fully male, meaning this is one of the conditions that causes a child to be born “intersex,” with neither clearly female nor male genitals. This situation can be caused by several things in addition to CAH and in fact intersex babies are more common than redheads, but I digress.
I grew up aware of what both low and high cortisol looked like as at various times, she was under or over medicated. For example, in her first grade picture, she looks thin and pale, which is Addisonian, whereas in her second grade picture, she has a moon face and is ruddy, more a Cushingoid look.
So when I developed the symptoms of “adrenal fatigue,” I recognized them. Though my morning cortisol was “in range” on the ridiculously large range, I badly failed an ACTH-stim test, and when I did the diurnal saliva test, I was low at every time point.
I also recognized a lot of the advice about “adrenal fatigue,” both diagnosing and treatment, to be utter nonsense.
I have called what I had “adrenal insufficiency” as it wasn’t bad enough to be called Addison’s, or late-onset CAH (which siblings often develop), but it was beyond a simple disordered circadian rhythm. And as noted, “adrenal fatigue” is often dismissed by physicians, and I’m not too fond of the way the term has been misused myself.
If you suspect adrenal issues based on a list of possible symptoms, my advice to you is to eat a heck of a lot of sea salt and take vitamin C. These things support the adrenal glands and may well totally fix minor symptoms and are unlikely to harm you.
A good choice would be either Anna’s or my electrolyte drink recipe.
Sleep is also important too, being in bed by 10 PM and staying there until at least 6 AM can correct quite a number of issues with circadian rhthym, as can getting sunlight directly on your skin every morning.
Supposedly, quitting caffeine is extremely helpful also, but I wouldn’t know about that as I never did it. 😉
Testing
How do you know if you have adrenal “fatigue”?
I do NOT recommend any other adrenal support medications prior to testing.
First, adrenal glandular supplements are often made from the entire gland, rather than the adrenal cortex, and thus contain adrenaline as well as cortisol, which can easily make you worse. Unless you’ve had a near-death experience, you don’t need adrenaline.
Second, the various herbs and adaptogens do different things. Some raise cortisol, some lower cortisol, some make cortisol last longer in the body effectively raising it hours later. If you don’t know exactly how your circadian rhythm is screwed up, trying to treat it can easily screw you up worse.
In my opinion, anything beyond salt and vitamin C can make you very much worse unless you get very lucky.
Furthermore, if you’re on anything other than general support for your adrenals, you can’t get accurate diurnal saliva results and figure out exactly what needs to be corrected.
Recovery from Adrenal Fatigue
What to do about it – a rational approach
Discussing exactly what treatments work for different patterns is beyond the scope of this article. I was involved with a group for a while, where I learned about the various rhythms, treatment options, and later was a mod myself for a couple years.
The group I was involved with deals with both adrenal and thyroid issues (which can affect each other) and can be accessed from their web site here The RT3 Adrenals website.
The protocols for testing adrenal function are on their site and if you join the group and post your test results, they will be able to advise you.
An Adrenal Crash is no fun at all
If cortisol drops much below what your body considers appropriate and does not respond to ACTH, your body may produce adrenaline instead, as it considers the inability to respond to stress to be an emergency situation.
This can lead to one of two scenarios, the first where you produce low levels of adrenaline regularly, thus disrupting sleep while not having enough cortisol to get out of bed, which I can tell you is not a fun situation AT ALL.
But it can also lead to a surge of adrenaline, in which you feel and react as if you are in a life-and-death situation. So your husband doesn’t wipe crumbs off the counter and you feel like your life has been threatened and overreact ridiculously; I tell you, the girly hormones have nothing on adrenaline for making you rather batshit crazy.
Finally, you can have an outright cortisol crash, in which you not only go rather nuts, but also wind up nauseous and puking. A crash will take days to recover from, even if you are taking cortisol replacement. It is extremely fatiguing and getting the cortisol not only into the cells, but into the mitochondria, and resetting the damage, just takes a few days. Best thing to do in that situation is just rest until recovered.
Adrenal Fatigue Diet
keto, but no fasting
So I will say something controversial for me, proponent of a ketogenis diet and fasting for reversing diabetes (and myriad other ills caused by insulin resistance): if you suspect adrenal problems, I do not think you should fast, not even intermittent fasting, let alone extended.
Fasting is a stress, moreso if you have a lot of detoxing or healing to do. You need to get adrenals sorted *first* and then add fasting, else you risk an adrenal crash, which I’m telling you, you do NOT want.
Keto itself is fine and preferable; it will slow the progression of insulin resistance while you sort your adrenal situation, and then you can add fasting to your regimen to reverse it.
How I Reversed My Adrenal Insufficiency
I was on steroids for years due to my adrenal insufficiency and with the assistance of my endocrinologist, attempted to wean shortly after I began ELAB.
My hypothesis was that if reduction of liver fat reduced insulin resistance and reduction of pancreative fat improved beta cell function, thus reversing diabetes, as Dr. Fung had said, perhaps reducing kidney fat could improve adrenal function.
Of course, I am an n=1 experiment, and thus don’t have enough data to support my hypothesis specifically, but I weaned prednisone very successfully over a 3-month period, with intermediate testing to make sure I was doing OK as I went along.
When I saw the endo again, I mentioned that I seemed fine off steroids entirely, but expected I might need hydrocortisone occasionally for stress-dosing. She suggested we find out and did a sort of half ACTH-stim test, gave me a shot and tested cortisol an hour later. Mine was off the charts, proving that my adrenals could not only handle daily stress just fine, but even extreme stress.
There can be a LOT of reasons adrenals can be messed up though, so my experience is not necessarily indicative of anyone else’s.
And while I was a naughty girl and began with a long, unsupervised fast, contrary to Dr. Fung’s advice, just testing bG and BP as I went alone, even I didn’t have enough balls to wean steroids without my endo’s advice, assistance and testing.
I’ve *had* adrenal crashes and would do rather a lot to avoid ever having one again.