They tell me I was born, but I don’t remember much about that. At age 5, I had a tonsillectomy, which was an extremely common surgery back then. Generally, I had a history of severe earaches in early childhood; I was in an ER nearly annually. At age 13, I broke my left arm due to a roller skating accident. At 19, I broke a finger when a car hit me and knocked me off my moped. It was a pretty uneventful childhood as far as medical issues go.
I gave birth to my daughter when I was 21; I was what was then considered borderline diabetic based on a GTT. The standards have changed significantly since then; today, I’d have been diagnosed with gestational diabetes and likely been on insulin throughout the pregnancy. Heck, back then they didn’t even test you unless a family member was diabetic; my father was.
At age 27, I was in graduate school when diagnosed with T2 diabetes. Rapidly realizing that the ADA’s recommendations were just stupid, I went to my research library and looked up how bG changes with varying macronutrient ratios of meals for normal people, T1s and T2s (we didn’t have bG meters back then; it was equipment only doctors had.) I invented a rather low-carb diet, but not understanding anything about circadian rhythms, concluded I should be eating a small dose of carbohydrate, a medium dose of protein and a larger dose of fat every 4 hours around the clock to keep bG as steady as possible.
Within a few years, I’d discovered I didn’t like waking up throughout the night to eat a meal that had been sitting out on my nightstand, and discovered the work of folks like Dr. Robert Atkins, Drs. Michael and Mary Dan Eades and most importantly, Dr. Richard Bernstein, a T1 diabetic who treated all diabetic patients, regardless of type, with a very low carbohydrate diet.
Other than the diabetes, my 20s and 30s medical history was not much more eventful than my childhood. I had a bad Pap smear, a surgery to fix that, then a repeat performance with a second surgery. Later, a benign growth was removed from my vocal chords.
Meanwhile, bG meters became commonly available. I learned things. I learned if I kept my net carbs under 50 g/day, my bG stayed relatively normal the vast majority of the time. I learned if I had a cheat meal, my bG would bounce back within a day, whereas if I had an entire cheat day, it’d take 3 days for my bG to normalize.
I attempted to use metformin several times, but after a few months, I’d begin to get what I then called fatigued and quit. Given that I was working a salaried position, 50-60 hour weeks, and raising a child by myself, my notion of fatigue was very different than what it is today! Of course, this was before we realized that metformin depletes B-12.
Then Actos and Avandia came along and every doctor wanted to prescribe them to every diabetic. I read about them, disapproved of their mechanism of action, and thus began my long history of arguing with my doctors. These drugs work by increasing the number of adipocytes in the body, which can then clear bG (adipocytes conveniently being cells that do not become insulin resistant). That was my personal objection, but it turned out these drugs cause fatal liver failure and heart disease, so are not a good thing.
But this was all OK, as my bG stayed pretty good for most of two decades just by not eating hardly any carbohydrate.
During my 40s, my perimenopause coincided with my daughter’s puberty, and all hell broke loose for a few years. Mother nature is quite a bitch having these things occur simultaneously, as if one woman being batshit crazy at a time isn’t bad enough! Our issues eventually resulted in a rather severe depression on my end, including a brief hospitalization for such. But I hit menopause and she grew up and turned out to be a decent human being, so that was behind us.
Towards the end of my 40s, I had a benign lump removed from one breast. And then one day, I called my daughter to take me to the ER because I was in horrific pain. I was admitted to the hospital with acute pancreatitis. I am a worse patient in a hospital than in a doctor’s office; I had a conniption when they tried to hook me up to an IV glucose drip while my bG was over 300, more than double normal bG.
After a few days, I was better and released with the explanation that this event would not affect my diabetes at all and had nothing whatsoever to do with diabetes. Though I understood T2 to be primarily a liver disorder, I had a bit of difficulty understanding how the pancreas had just had this little temper tantrum and it had nothing to do with T2 diabetes.
Well, it had a bit of an effect. My bG never went below 300 for nearly a year. I went very strictly low carbohydrate; my bG didn’t budge. I went no carbohydrate, just meat and eggs, it still didn’t budge. I fasted several days, and still my bG remained ridiculously elevated.
Low carb didn’t work anymore; I speculated that my body had become extremely efficient at gluconeogenesis. And I spent quite a number of years thereafter slightly confused about what to recommend to other diabetics; it HAD worked for nearly 2 decades, and then it didn’t. It seemed to me to be the best we had, but it obviously didn’t fix the problem.
So I went into denial. I didn’t have insurance anyway, so it was easy to postpone. And I knew if I went to a doctor, I’d be put on insulin; I was TERRIFIED of that. They *threaten* you with insulin, that if you are not “good,” you will *have* to go on insulin. (It turned out the shots hurt significantly less than all the finger-poking I’d been doing for years.)
And… I couldn’t fix my bG anyway, so what is with this low-carb stuff? What is the point? There is pizza in the world! And garlic bread! And pasta! It makes no difference whatsoever if I make real lasagna with noodles instead of my low-carb version. I can’t fix this anyway.
It turns out if you are too chickenshit to go see a doctor because you suspect they will prescribe insulin and you try to catch up on all the crap you didn’t allow yourself to eat for nearly two decades, a little thing called a myocardial infarction can happen to you. At age 45, I got a big one and have been disabled since.
They attempted to clear the blockage with an angioplasty, but were unsuccessful, so I was scheduled for a robot-assisted CABG. The surgeon decided I was too unstable for the robot-assisted thing and cracked my chest open like a chicken breast.
I was told it would take me about 3 months to be back to work; so far it’s been 12 years.
At the beginning, I was mostly bedridden for a year and when a whole bunch of other fatigue-related things like Lyme disease and anemia were ruled out, I was diagnosed with ME/CFS.
My first attempt towards health was achieving very tight bG control with the assistance of other diabetics; learning to calculate my carb and protein ratios, then applying that to the calculated macros in each recipe I used, I could keep my bG very tightly controlled, usually fasting under 100 and postprandial under 140. I achieved an A1c under 6% several times, the ultimate goal of a diabetic!
And I must admit, that tight bG control was not sustainable; you have to spend as much attention on food as someone with a severe eating disorder, but without the psychological illness to provide motivation. There were times I just got burnt out on the whole thing and lived on protein shakes for a week just so I could just take insulin the same way every day without all the calculations. I looked back fondly on the time when all I had to do was eat low-carb to control bG.
But I was still mostly bedridden, unable to do much more than a shower on any given day. Tight control of my bG was difficult and not paying dividends. My life at the time was like this: say I have a doctor’s appointment next Friday. The previous Saturday, I would do grocery shopping, then rest up for 2 days, not getting out of bed. Tuesday, I’d cook enough food for a week, then rest again on Wednesday. Thursday, I would shower thoroughly, not having done so for nearly a week, in preparation for my appointment on Friday, then spend the following weekend in bed. This is how few spoons I had; it took over a week to manage a doctor appointment.
Stuck in bed so much, what I could do was research. I tried various medications that I thought would fix me, numerous supplements, and even several diets: gluten-free, dairy-free, GAPS, even a raw milk diet. But I’m getting ahead of myself; this was over the course of several years.
Two things I tried *did* help.
After failing an ACTH-stim test and then doing a diurnal saliva cortisol test, I discovered I had severe adrenal insufficiency. Getting on hydrocortisone (and later dexamethasone and prednisone) gave me a huge boost in energy, allowing me to get up nearly every day. Paradoxically, while bedridden, I had severely disordered sleep and got very little; treatment for my adrenal issues also straightened that out.
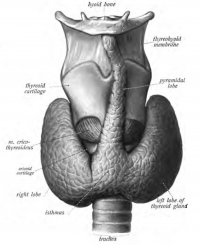
Secondly, I discovered I had extremely elevated reverse T3. Treatment with T3-only meds resulted in another surge of energy about 2-3 months in.
I even started thinking maybe I could handle a part-time job. But the fatigue still varied a lot; I wasn’t sure if I could handle it on an ongoing basis. Though these two medications made me better, they did not make me “all better.” I still had to count my spoons carefully and spend them wisely.
And I was still deteriorating. By the age of 53, I had severe lymphedema in my legs and feet. Unfortunately, fast-acting insulin did a real number on me, blowing my feet up past the point of not wearing shoes all the way to not being able to stand. I saw a physical therapist who taught me to do bandaging and later prescribed $300 stockings, but I couldn’t reach to do these things myself. Eventually, she prescribed a lymphapress, but due to insurance snafus, it would be a couple years before I actually got it.
Meanwhile, since I couldn’t tolerate bolus insulin and basal wasn’t doing the job, my PCP sent me to an endo, who prescribed an SGLT-2 inhibitor. Always suspicious of new drugs, I read all the research available at the time and concluded these drugs were OK.
They are NOT. Less than a year later, I had an ER doctor telling me I had DKA, which I explained I could not have that because I was a T2; only T1s get DKA. And he told me that these drugs had been shown to cause DKA in T2s! So I nearly died, spent several days in ICU with all possible electrolytes dripping into both arms. I also had cellulitis, an infection in my legs, due to the lymphedema. Fun times!
Obviously, I dropped the SGLT-2 inhibitor pretty rapidly. But about a year later, I had another newly-discovered side effect: necrotizing fasciitis.
This has been in the news lately, in which people are picking it up at beaches and whatnot; those cases are a specific virulent bacteria. The type I had was just ordinary bacteria who decide they’re on spring break and have a party in the subcutaneous fat.
In either case, this is life-threatening. I apparently lost my mind, though I was conscious and talking and such, I have no memory of what occurred; I simply lost 6 weeks of my life. What occurred was this: I behaved more and more bizarre, eventually an ambulance was called, I was rushed to the hospital and then helivaced to the Shock and Trauma unit at University of Maryland where 3 emergency surgeries were performed back-to-back resulting in a chunk of my thigh being removed that Steve tells me was as large as a sheet of paper and as deep as a ream.
Lots of other fun things happened as well, I was intubated (which I apparently hated), nearly died a couple times from low BP events (I generally have hypertension as do most diabetics), had a pulmonary embolism, had several stents put in the same leg they’d operated on because 3 of my toes went black, was fed through a tube in my nose for weeks. Again, I nearly died several times.
And honestly, for some time, I wished I had. When I came to, I was still somewhat delirious, and found myself with mittens on my hand to prevent me removing tubes like the one down my nose and tied to the bed with an alarm attached to me to notify the nurse’s station in case I tried to escape.
The alarm was not necessary; I couldn’t move. As my various restraints were removed, I discovered I could not even change position in the bed; when I slid down, I had to ring for assistance to shift my position. And there were the twice a day dressing changes, during which the muscles of my leg actually fell out and had to be shoved back in and I was *positive* they weren’t giving me real narcotics because it just hurt so damned bad.
When I got out, first I went to rehab where I learned to stand and walk again (took over a month) and then home where I had a physical therapist at home until deemed well enough to go to outpatient physical therapy. When fired by my insurance because I wasn’t improving enough, I could walk on flat surfaces, but needed a stick or cane for curbs and uneven ground and could not get up from the floor.
A few months at home, I woke one day to discover the one toe that had never healed entirely had fallen off. And after about a year of seeing the wound doctor, I was sent to a plastic surgeon to get a graft for the bit of my leg that didn’t heal.
And it turned out about a year later, necrotizing fasciitis was added to the black box warning for SGLT-2 inhibitors. Oh, and increased risk of amputation, though I was lucky to only lose a toe. I had hit the trifecta: DKA, necrotizing fasciitis and amputation – all from this drug.
Life went on and eventually, I was glad I still had one. I finally got my lymphapress, had a return of rT3 issues and went back to T3-only meds, weaned off of oxycodone, had some rotator cuff issues that were fixed with another round of physical therapy.
And then in the summer of 2018, I woke unable to breathe, and called 911 and spit out my address. In the ambulance, they gave me oxygen and I seemed to recover. At the hospital, they gave me a nebulizing treatment, said I had COPD, was maybe having a heart attack, and suggested admitting me. I declined.
A few days later, it happened again, and this time, my stubbornness about the hospital waned; even after ER treatment, I still could not breathe. I was admitted, given large doses of IV Lasix, and once the fluid cleared, I could breathe. I had congestive heart failure, when your lungs fill with fluid and thus can’t provide oxygen to your heart.
I was later tested by a pulmonologist and it was determined I did not have COPD, but I was on a bunch of breathing stuff, a nebulizer and 2 inhalers, for several months before we determined I didn’t need any of it.
Nothing awful happened for another year, I was muddling along. However, I was rather certain I was going to die soon and wasn’t particularly bothered by the idea given that my entire life involved sleeping, sitting in front of my computer, shopping once a week and the occasional doctor appointment. I woke every day and thought about what I HAD to do on the way to the john; somewhat disappointed that I’d woken up again.
In April 2019, I went on a pilgrimage to my hometown as that seemed a fitting thing to do; my best friend, Pete, told others when he saw me that he didn’t expect me to last a year.
In June of 2019, I got a case of CHF again. Determined NOT to go to the hospital, I doubled up on Lasix at home. It took weeks to be able to breathe well again, during which time I could barely stay awake 3 or 4 hours, and when I forced more, was too brain-fogged to even read or respond to people speaking to me. I began to realize that I might NOT die, I might instead wind up in a nursing home; I couldn’t even nuke meals prepared by my home health aid earlier in the day. I ordered a tank of nitrogen and began practicing making exit bags; I’m not going to a nursing home; this is not negotiable.
But after a couple weeks, my lungs cleared, and then I focused heavily on potassium and using the lymphapress until I could get back in my shoes. By July, I was doing much better, I could manage to sit at my computer and read most of the day again. So… I was still probably going to die soon, but no hurry as I could manage at home with home health aid assistance, so no nursing home threatened.
And then… I had an epiphany.