So after I had managed to wean off prednisone, my next thought was I wanted to wean off liothyronine, T3-only meds, which I was taking for what I call thyroid resistance.
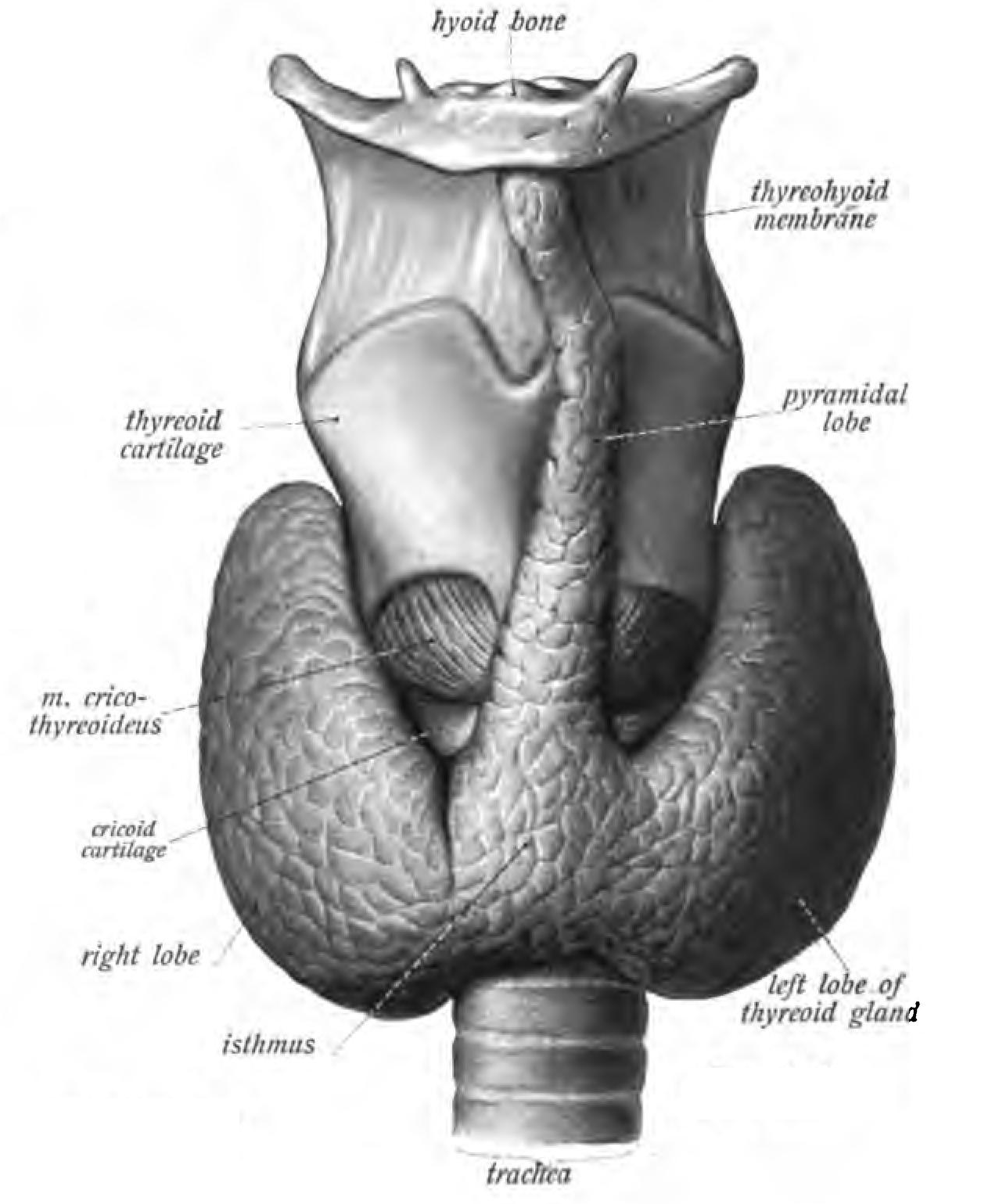
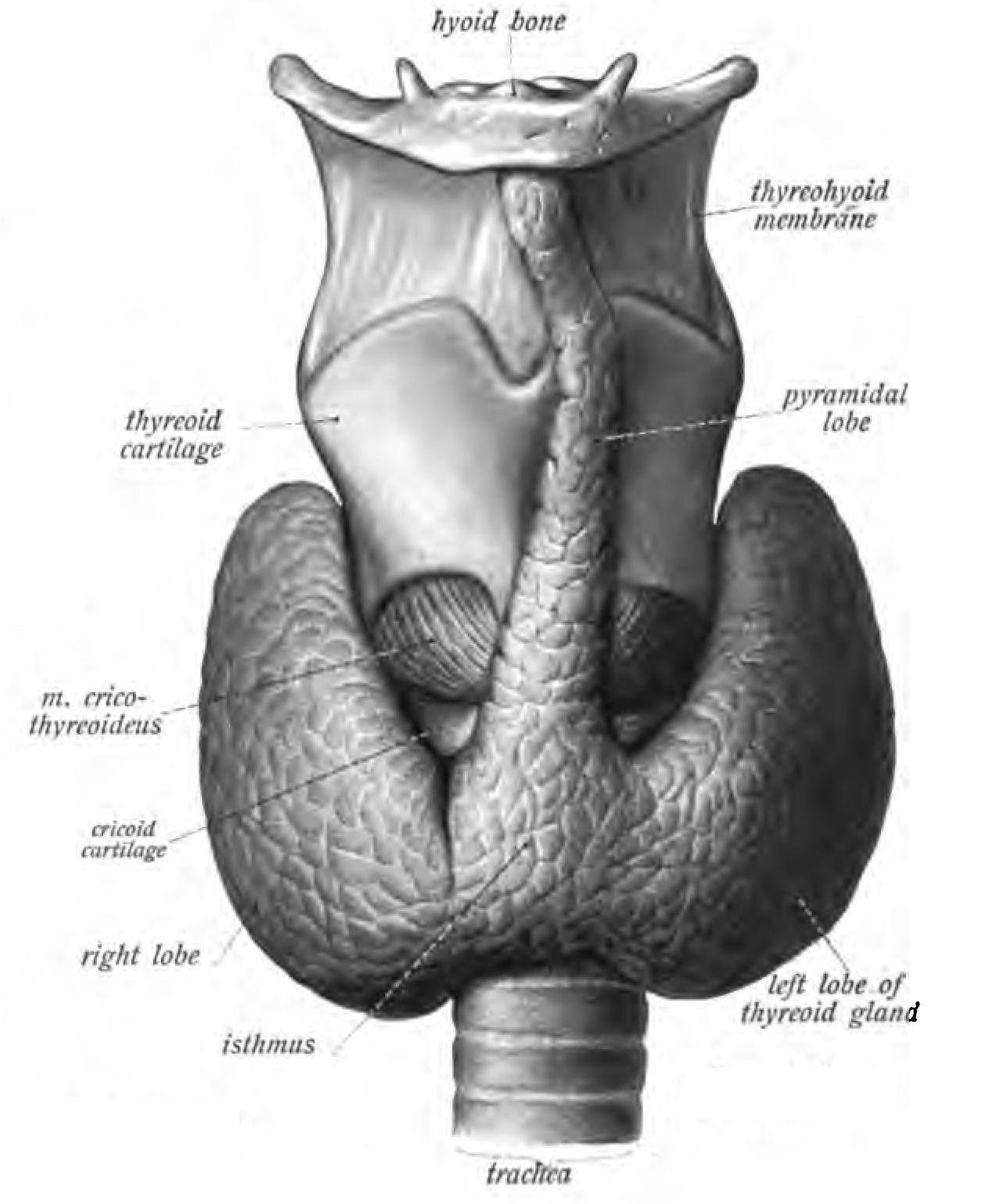
Basically, the point is this: mostly, the thyroid makes T4, so named because it has 4 iodine molecules attached. T4 has to be converted to T3, which is the active hormone. However, sometimes things go awry and instead T4 is converted to rT3, reverse T3.
Reverse T3 fits into the same cell receptor as T3, but what it does instead of ramping up metabolism is slow it down; rT3 is what causes hibernation in bears.
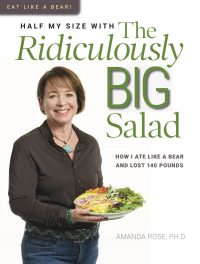
While I did learn to eat like a bear, sleeping like one was not ever desirable!
my original treatment and how to get help
Treating my adrenal insufficiency and thyroid resistance had helped me a great deal; it relieved much of my symptoms of ME/CFS.
If you have, or suspect you have, adrenal or thyroid issues, I highly recommend the adrenals/rT3 group, which can be accessed via their web site. Once you’ve joined, they can advise you regarding your lab results, what they mean and what to do about it.
I personally do not recommend keto and fasting until your adrenals and thyroid are sorted; you’re likely to have a “crash” and become very ill.
On the other hand, both of mine healed via keto and fasting.
It’s important to not that there was nothing wrong with my adrenals; my issues had to do with the HPA axis. Similarly, there was nothing wrong with my thyroid gland; my liver was just producing rT3 out of the T4 my thyroid produced. While I expect that medications can often be reduced as the body heals via autophagy, if there are actual issues with the glands, it’s unlikely you’ll be able to wean.
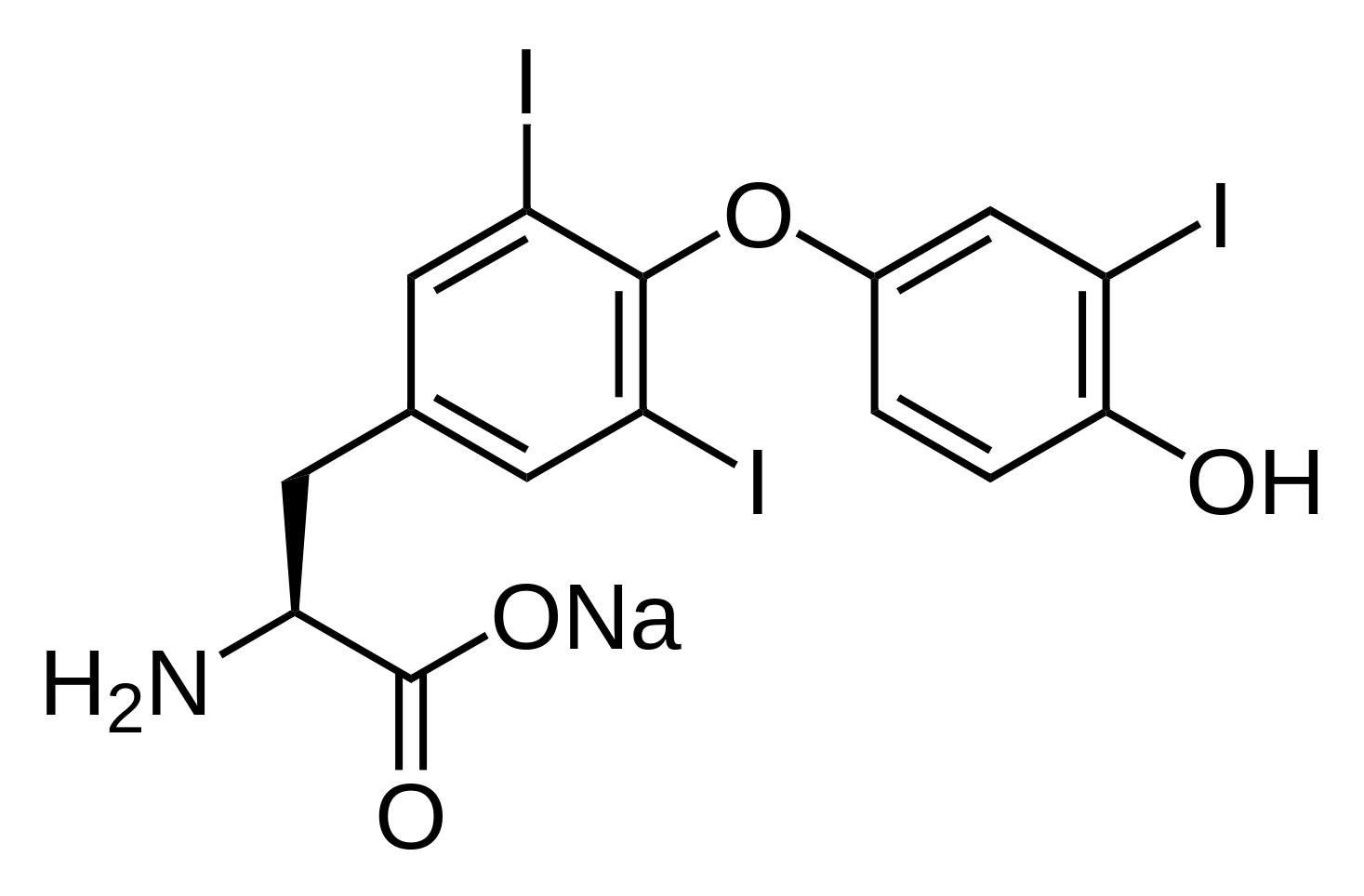 molecular structure of liothyronine, note the 3 iodine atoms
molecular structure of liothyronine, note the 3 iodine atomsReverse T3 issues are diagnosed via comparing the amount of rT3 and FT3 on blood work. Given that many doctors do not run these tests when thyroid issues are suspected, many patients go undiagnosed and untreated.
My endo didn’t entirely agree with me treating my thyroid resistance via T3-only meds. She said when rT3 was high, it was “euthyroid syndrome” and she believed it was part of the healing process. I began seeing her shortly after I’d had multiple surgeries for necrotizing fasciitis, had done a stint in rehab to learn to stand and walk again, and was seeing a wound doctor for the gaping wound remaining on my leg. As such, her explanation was believable and I weaned down to 37.5 mcg liothyronine/day.
But I stopped there years before I began my recovery, as trying to go lower meant I couldn’t stay awake long enough to shower, eat, grocery shop and make it to my myriad doctor appointments. While I could buy the idea that my body needed to rest to recuperate, I required minimal functionality; sleeping over 20 hours/day just wasn’t acceptable to me.
So I remained on T3-only meds for a number of years, which she said was OK as long as my TSH didn’t actually get to zero; she didn’t want my thyroid entirely suppressed. Given that part of the purpose of T3 meds is to suppress the thyroid’s production of T4 so no more rT3 can be made, this is contrary to the entire theory of correcting rT3 issues.
But it was a compromise that she and I agreed to and I secretly was pleased whenever my TSH came back very low.
confusing labs
At the same visit when we discussed weaning prednisone, I asked the endo to run an FT3 and rT3 and she agreed; she wanted the TSH the same as always. I figured if my labs were good, I could proceed with weaning T3 meds after I finished weaning prednisone. I had a secret hope that my endocrine system might be able to work without me micromanaging it.
I was still on 30 u insulin and 5 mg pred when the blood draw was taken; my labs were neither good nor bad, just terribly confusing.
As previously mentioned, it is the ratio between FT3:rT3 that is indicative of issues; <20 is considered a problem. This is because they compete for the same cell receptor; if rT3 is bound and slowing metabolism, it excludes T3 from binding and raising metabolism.
My ratio was good, because my rT3 was very low. But my FT3 was *also* below range. This made no sense to me, thyroid patients generally feel best with FT3 near the top of the range.
How could I feel as well as I did with so little T3?
I searched my known resources for advice. I didn’t receive anything useful.
I did test my DATs (daily average temperatures) and they were fine; my averages stayed consistent and I hit 98.6 every day.
Others insisted I must feel terrible with an FT3 that low, but I was *in* my body and felt better than I had in over a decade.
When I saw the endo again, she said my TSH was OK, which was her entire measurement of how I was doing.
So I had to decide on my own whether to try to wean liothyronine or not as I had no data or advice I considered reasonable to base the decision on.
I decided the FT3 test must be wrong; I simply felt too well to not have plenty of T3. And I freely confess that my decision was largely emotional; I *wanted* to be free of exogenous hormones.
So… after I’d finished weaning the prednisone with such spectacular results, I decided to try weaning liothyronine too.
The endo and I discussed a weaning schedule, and I must admit, I went much more slowly than she had suggested, checking temperatures and just seeing how I felt as I proceeded. She also wrote more TSH labs, but I found those irrelevant; I cared about my temperature and how I felt; but my endo and I had an understanding; she wrote the labs I wanted and I bled for the ones she wanted.
I began weaning in November 2019; by the time I saw the endo again in January 2020, I was off it. It was much more difficult than weaning prednisone had been.
My next visit with Dr. Yan amazed both of us!